Basal MET phosphorylation is an indicator of hepatocyte dysregulation in liver disease
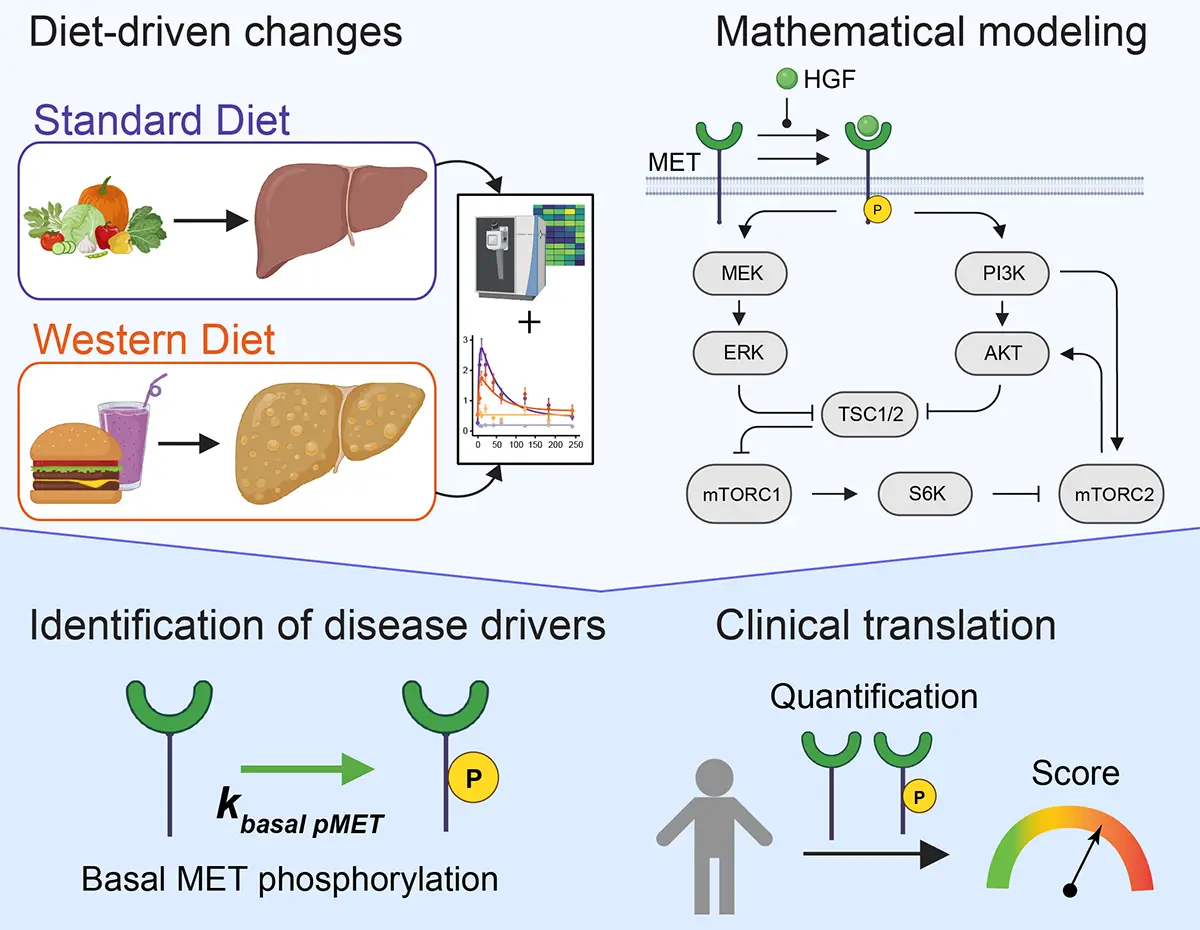
Graphical Abstract
Primary hepatocytes from a preclinical mouse model fed with high-sugar and high-fat diet are used to develop a data-based mathematical model that identifies the basal phosphorylation rate of the tyrosine kinase receptor MET as the main dysregulated parameter driving fatty liver disease.
An increase in phosphorylated MET and a strong downregulation of the PI3K-AKT pathway in response to hepatocyte growth factor (HGF) stimulation are hallmarks of primary hepatocytes derived from mice exposed to a high-fat and high-sugar “Western” diet.
Dynamic pathway modeling of HGF signal transduction combined with proteomics identifies elevated basal MET phosphorylation rate as the main driver of altered signaling and increased proliferation.
Model-adaptation to primary human hepatocytes reveals that patient-specific variability in basal MET phosphorylation correlates with patient outcome after liver surgery.
Abstract
Chronic liver diseases are worldwide on the rise. Due to the rapidly increasing incidence, in particular in Western countries, metabolic dysfunction-associated steatotic liver disease (MASLD) is gaining importance as the disease can develop into hepatocellular carcinoma. Lipid accumulation in hepatocytes has been identified as the characteristic structural change in MASLD development, but molecular mechanisms responsible for disease progression remained unresolved. Here, we uncover in primary hepatocytes from a preclinical model fed with a Western diet (WD) an increased basal MET phosphorylation and a strong downregulation of the PI3K-AKT pathway. Dynamic pathway modeling of hepatocyte growth factor (HGF) signal transduction combined with global proteomics identifies that an elevated basal MET phosphorylation rate is the main driver of altered signaling leading to increased proliferation of WD-hepatocytes. Model-adaptation to patient-derived hepatocytes reveal patient-specific variability in basal MET phosphorylation, which correlates with patient outcome after liver surgery. Thus, dysregulated basal MET phosphorylation could be an indicator for the health status of the liver and thereby inform on the risk of a patient to suffer from liver failure after surgery.
